“…brute reason is quite unbearable. There is something quite unfair about its use. It is hitting below the intellect.”
Oscar Wilde
My more recent posts have addressed some of the complexities that arise further on in the recovery process (beyond eight months or so) and now I’ll get back to a few posts on some basic problems that plague those contemplating recovery or in those early stages of recovery from an eating disorder.
I actually mean to be a bit caustic in this post. Caustic substances are corrosive. I would like to undermine the lies built up by economically interested parties that hide all the underlying truths regarding “obesity” and disease. I am under no misconceptions that I will succeed of course.
But I would like to assure all readers that the tone of this post is not directed at those of us who have accepted the lies at face value thus far (not as if I cannot count myself among them in the past), but I hope I don’t spare those who are purposefully spreading the lies for financial gain.
Weight Set Point Theory Is Not A Theory
Does everyone understand that weight set point theory does not mean "theory" in an English language sense, but in a scientific sense?
It is a fact our bodies do maintain an optimal weight very closely 1,2,3,4,5,6,7,8,9,10 Human height, weight and body mass index are highly heritable. Classic twin studies indicate heritability of 0.80, 0.81 and 0.84 respectively. 11
However it is scientifically undefined at this point how our bodies actually manage to achieve that feat and not that our bodies may or may not have an optimal weight set point.
Our bodies have an undisputed optimal weight set point. But until we know how the body does that, then in science we have a working hypothesis against which we can test the theory’s accuracy. The theory being, the body has mechanisms by which it maintains its weight within a very close range.
Here is the actual scientific weight set point theory defined:
“In adult individuals body weight is maintained at a relatively stable level for long periods. The set-point theory suggests that body weight is regulated at a predetermined, or preferred, level by a feedback control mechanism.
Information from the periphery is carried by an affector to a central controller located in the hypothalamus.
The controller integrates and transduces the information into an effector signal that modulates food intake or energy expenditure to correct any deviations in body weight from set-point.
Evidence for involvement of various factors and physiological systems in the control of food intake and regulation of body weight and fat are reviewed within the context of a control model.
Current working hypotheses include roles for nutrients, dietary composition and organoleptic properties, hormones, neural pathways, various brain nuclei, and many neurotransmitters in the regulation of food intake. It is concluded that regulation of body weight in relation to one specific parameter related to energy balance is unrealistic. It seems appropriate to assume that the level at which body weight and body fat content are maintained represents the equilibria achieved by regulation of many parameters.” 12
To reinforce the concept:
That human beings have an inherited optimal weight set point = FACT.
How biological systems maintain that inherited optimal weight set point = NOT FULLY UNDERSTOOD.
Can You Change Your Optimal Weight Set Point?
No. You can most certainly stay on a permanent restrictive diet but you have not lowered your inherited optimal weight set point, you've suppressed it. Notice how I so easily assume that by “change” everyone means “lower” their optimal weight set point? But in fact, you cannot raise your optimal weight set point permanently either. 9
Permanent restriction slowly catabolizes your body’s cells to make up the energy deficits you are creating through restriction. It’s a good way to generate progressive ill health but not a way to shift your inherited optimal weight set point. And think again if you want to assume that “maintaining” your weight below that which is your inherited optimal weight set point will mean cessation of catabolism and optimal health. In fact the catabolic pathways as well as adaptive thermogenesis are most likely contributory factors for the return to an optimal weight set point. 13,14,15,16,17 And don’t discount that your entire living system is suppressed when you are below your optimal weight set point. Those biological shutdowns are short-term survival mechanisms that are not sustainable long-term. 18,19,20,21.
Virtually everyone who attempts to adjust an optimal weight set point downwards (i.e. lose weight) will fail utterly within 2 years. And so, in an attempt to suggest better outcomes, the clinical definition used in the National Weight Control Registry for long-term weight reduction success is an intentional loss of 10% of total weight that is maintained for 18 months. 22
Another solid meta-analysis showed that the best-case outcomes for sustained weight loss (no matter the program involved) was to regain 77% of initial kilograms lost by year 4 or 5. And less than 50% of those enrolled were able to achieve that underwhelming result; the rest regained more than 77% of initial weight lost. 23 Even systematic review of programs that include exercise can only offer up the following tepid 1 year outcome: "The combined intervention also resulted in a 20% greater sustained weight loss after 1 y (6.7 kg vs 4.5 kg; z=1.89—p=0.058, 95%CI) than diet alone. In both groups, almost half of the initial weight loss was regained after 1 y." 24
Just let that sink in for a moment: both groups regained almost half of the initial weight lost in a year.
But wait, the National Weight Control Registry contained 2500 names of individuals who had lost an average of 33 kg and maintained that loss for five years. 25 Given that at least 90 million people would have been dieting in the US in 1995 (34% of its population* five years before the 2500 successful people were included in that registry), then actual long-term weight loss was successful for 0.003% of the population in the US at that time. [*that is the lowest percentage in the assessment range of somewhere between 34-50% of the population is dieting in any given year, source MarketData 2012].
Even when you use a diet drug such as orlistat, the weight regain is only half as much those using placebo in the two years following the restrictive attempt to lower optimal weight set point (randomized controlled trial-RCT). 26 And of course the FDA issued a health warning about orlistat (brand names Xenical and Alli) in 2010 regarding incidents of severe liver injury [FDA Drug Safety Announcement: Orlistat]. A thorough review of RCTs on weight loss maintenance had this weak endorsement to offer up:
“The results of the reviewed trials revealed that treatment with orlistat or sibutramine combined with dietary modification, caffeine or protein supplementation, consuming a diet lower in fat, adherence to physical activity routines, prolonged contact with participants, problem-solving therapy and the alternative treatment acupressure were efficacious in reducing weight regain after weight-loss treatment.” (emphasis mine) 27
Keep in mind that any weight set point adjustment is not biologically achieved here. You can run, you can diet, you can run and diet and you must keep that up in perpetuity to suppress your optimal weight set point by a spectacular 3-4 kg (6.6-8.8 lbs.). 28,29
About the only way in which a weight set point might permanently be changed without these pathetically unsuccessful, physically and mentally damaging ‘permanent lifestyle changes’ (and certainly has not been attempted with humans) is to create lesions in the hypothalamus (destroy brain tissue). 27 Still, given that we are already happy to mutilate stomachs, I cannot rule out the possibility that partial hypothalectomies might not become all the rage.
Your optimal weight set point is fairly static through adulthood, however it shifts naturally upwards between the ages (approximately) of 50-65 and then shifts naturally downwards into old age. And, very interestingly, this might be due to bone and muscle density changes associated with the natural aging process that signal the necessity of a shift upwards in fat mass, nudging the optimal set point, as a health protective process to ensure overall vitality into advanced old age. 30,31,32
But What About All The Obese People Out There?
As soon as it is roughly understood that a body can maintain its weight and it’s not seen as a theory as in “theoretically, faeries could exist”, then it is common to be puzzled about why fat people exist and in supposedly ever increasing numbers with ever increasing girth.
Warning: I am going to use the word “fat” a lot. If you need to breathe into a paper bag when faced with that word, then I suggest you have one nearby before you read further.
I will debunk this so-called obesity epidemic or crisis on three fronts:
- Reaching our optimal inherited age, height and weight is dependent on innumerable environmental and sociocultural factors that have not remained constant throughout history.
- "Overweight” is not a population-based concept. Weight and height exist on a natural bell-shaped curve graph of incidence across our populations.
- Obesity is not a disease. It is not a marker of ill health or lowered life expectancy. The chronic conditions that are weakly correlated with “obesity” exist at all weights and are more likely to cause death in those who are average or below average weight than those who are above average weight.
Heritable Traits: How They Work
Asking “Why are people getting fatter if weight is inherited?” is like asking “Yes, but if height is inherited, why are people getting taller?”
If you do not have optimal nutrition, nurturing, safety, protection from the elements and so on from birth, you will neither reach your optimal skeletal frame size nor optimal fat organ size. You will be stunted and underweight (relative to your optimum). Oh, and your life expectancy will be lower too.
When the human population was sparse and nomadic, humans appear to have had life expectencies of 70+ (assuming they survived their first five years of life and did not die a violent death). This estimate is arrived at from studying remaining nomadic tribes today, but of course ancient lifespans cannot be confirmed with any real degree of certainty in this way. 33,34
The heritability of life span exists only on a population-wide level and does not translate to a high familial heritability factor. Your grandmother could pass away at age 106, but that does not mean her progeny is going to inherit living to an equally grand old age. Age appears to have a familial heritability factor of between 0.35 and 0.50.
It is likely that life span is more of a species-specific trait. In other words, modern human beings have likely always been genetically coded to live about 85-92 years on average, just as chimpanzees can live about 35-41 years on average.
Life expectancy dropped precipitously when humans went agrarian. That happened for a variety of reasons: hierarchical distributions of food, exposure to pathogens in greater numbers, and crop failures. 35,36
Interestingly, during the so-called Dark Ages after the fall of the Roman Empire, human populations increased in height in Northern Europe and this was attributed to the more egalitarian use of resources and food at that time. Average heights fell from 173.4 cm in the early Middle Ages to 167 cm by the 17th century. It appears that the most plausible reason for this stunting was the uneven distribution of resources and food with increasing hierarchical oppression. 37,38
So your ancestor who lived at the beginning of the Industrial Revolution likely had all sorts of hidden potential for being taller and heavier that was not realized due to sub-clinical starvation and socio-economic stressors from gestation onwards.
In the past 25 years alone, teenagers have increased overall 1% in height and 4% in weight on average. In that same time period, life expectancy increased on average by 6 years in most developed nations, which in Canada translated to a 7% increase in life expectancy from 1980 to 2005 (National Statistics). Rather interesting correlations, no?
And why did our populations remain thinner and shorter than today, despite improved nutrition after the Second World War? Smoking rates— that coincidentally began declining 25 years ago.39,40,41 Smoking suppressed reaching optimal weight and generated massive spike in disease states. In fact cardiovascular disease and mortality rates have dropped with smoking rates despite the questionably touted correlation of weight and heart disease.
The majority is just getting too much optimal, early and good nutrition, care and safety to stay stunted, thin and short-lived.
Are we heavier than 25 years ago on average? Yes, and we are also taller and we live longer on average too. Poor us.
What Is Overweight? What Is Obese?
I talk about these issues in much more detail in the Fat Series but we know it’s a committed read to work through those concepts in depth.
Here is the short(er) version:
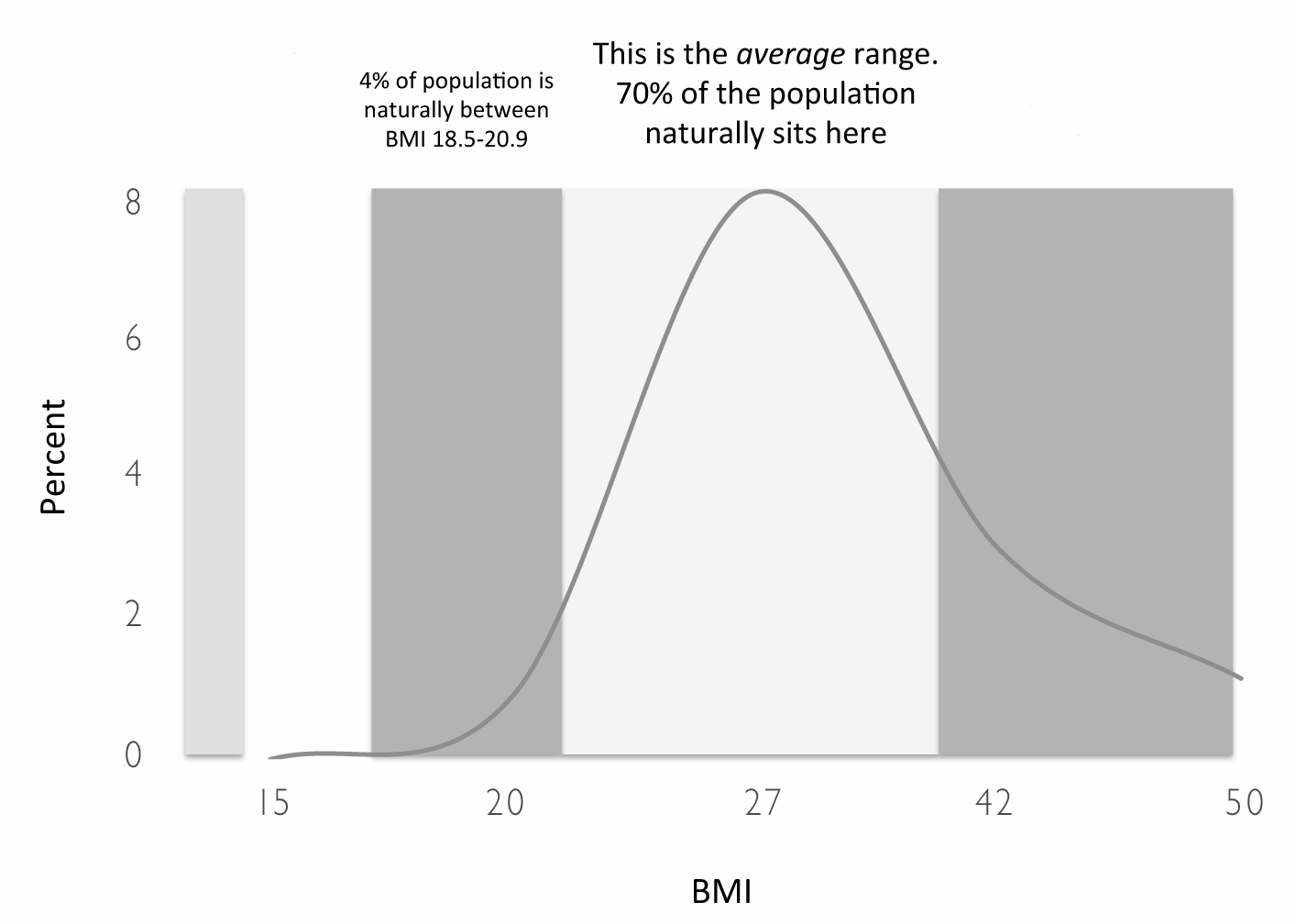
- Does the above image make sense? That curve above includes approximately 7 billion human beings and it means the majority of us naturally has a body mass index (BMI) of 23-31.
- Can you see, by looking closely at that line, where the sick people are? No? That’s correct. Because there are both ill and healthy people scattered all the way along that line.
- Weight is not a measure of health. Weight is not a predictor of sustaining your health either.
- When the National Institutes of Health convened a Panel on Obesity in 1998, the committee members identified cut-off points that would denote increasing risk of ill health and early death (morbidity and mortality risk) based on BMI.
- That’s how you found out that being BMI 25 is “overweight” (or even pre-obese for the truly deterministic) and being BMI 30+ is “obese”. The report suggests that people on the right hand side of the peak of that line are either sick and dying, or at risk of being sick and dying.
- Here’s what you don’t know about how the POO arrived at these pronouncements (couldn’t resist an acronym like that for Panel On Obesity):
- The Chair of the Panel received or receives research and grant support from: Novo Nordisk (new weight loss drug) and Merck (new weight loss drug). He additionally acts as a paid consultant and advisory board member for: Novo Nordisk (diabetes mellitus, obesity), AstraZeneca (obesity), McNeil Nutritionals (non-caloric sweeteners) and Weight Watchers (obesity).
- In fact 8 of the 9 members of the POO have, or had, ties to the weight loss industry. Those conflicts of interest were not published in the NIH POO report but were uncovered by two journalists: Kitta MacPherson and Ed Silverman. 42 For more recent conflict of interest issues for the Federal Guidelines Panel on Obesity, you can check out this New York Times Graphic.
- The two primary peer-reviewed published data upon which the POO based their pronouncements that BMI correlates with increasing health risks and early death are not credible. The first does not confirm obesity as a contributing factor for early death and the authors have actually made attempts to stop having their data misrepresented as it has been by the POO [NEJM, 1999]. The second study failed to control for activity levels, genetic pre-dispositions, presence of other serious illnesses, history of weight cycling, use or misuse of diet drugs, use of bariatric surgery, etc.
- As such, the POO has no data upon which to base the BMI cut-off points as credible identifiers for increased health risks.
- The POO has serious (and unpublished within the report) conflicts of interest and has no science upon which to relay to all of us that BMI 25+ is a health risk or that BMI 30+ is a death sentence.
- The Chair of the Panel received or receives research and grant support from: Novo Nordisk (new weight loss drug) and Merck (new weight loss drug). He additionally acts as a paid consultant and advisory board member for: Novo Nordisk (diabetes mellitus, obesity), AstraZeneca (obesity), McNeil Nutritionals (non-caloric sweeteners) and Weight Watchers (obesity).
If you inherit an optimal BMI of 41 then there is absolutely nothing in that number that tells you that you are sick and dying. Not one thing.
If you inherit an optimal BMI of 18.5 then there is absolutely nothing in that number that tells you that you are healthy and immortal. Not one thing.
Obesity as Disease
Fat people are sick people. The POO tells us it is so and therefore we accept the claim as fact.
I don’t want to re-hash all the data I have already amassed within the Fat Series so again go read it if you want to be sure of the details.
Here are the high points:
- The relative risk increase of diabetes mellitus Type II onset with obesity is equal to that of the relative risk increase of diabetes mellitus Type II onset with a psychiatric disorder. 43
- In one study Type II diabetes mellitus prevalence in obese vs. nonobese patients with coronary artery disease 54%% and 34% respectively. In yet another study, 60% of the over 35,000 people studied over an 8 year period had diabetes and were not obese. 45
- And while diabetes mellitus Type II is confirmed to be the same chronic condition in both obese and non-obese patients 46, obese patients with diabetes have better morbidity and mortality outcomes than their non-obese counterparts. 47
- Diabetes is also over-diagnosed in our society due to fasting blood glucose cut-off point changes that lack evidence to support the new cut-off. 48
- While sleep apnea, hypertension and cardiovascular disease are correlated, 50% of those with sleep apnea are not obese. 49
- Angiographic studies repeatedly show fattest men and women have the cleanest arteries and an analysis of 23,000 sets of coronary vessels confirmed there was no relationship between heart disease and body fat. 50,51
- Being BMI 25-29.9 generated 86,094 fewer deaths than expected when reviewing NHANES data. Therefore the “overweight” category has the lowest mortality rate. 52
- Correlations of obesity and certain cancers fail to rule in or out the presence of inflammation and insulin resistance and therefore misconstrue correlation with causation. 53
- And while increased body weight is associated with increased death rates for all cancers 54, these results may be attributable to obese patients receiving both inadequate diagnostic testing and in particular intentionally inadequate chemotherapeutic dosing. 55
- “Among US adults, there is a high prevalence of clustering of cardiometabolic abnormalities among normal-weight individuals and a high prevalence of overweight and obese individuals who are metabolically healthy.” 56
Not only is being larger than average not a disease, it is not the cause of disease either.
But There ARE Sick Fat People
Yes there are. There are sick fat, average and thin people everywhere. There are even dying fat, average and thin people everywhere too.
There are sick and dying blue-eyed people, red-haired people, tall people, brown-eyed people, and even people with eyes that are different colors as well.
Shockingly, there are also healthy 600 lb. people out there. And even more shockingly, there is a very good chance (given the readership of this site is disproportionately dealing with eating disorders) that that 600 lb. person is actually very much healthier than you are too.
But there is unequivocally one death per person. No way around that one. To paraphrase Nortin Hadler: “By age 50 there are several things in you that are already vying to be listed as proximal cause of death when your time eventually comes.”
Getting sick is not preventable through diet. Reversing the symptoms and damage associated with some chronic illnesses can sometimes be achieved through dietary changes. And unfortunately almost everyone thinks those same dietary changes can prevent the illness in question.
I’ve talked about this fallacy in thinking in many a thread on the forums of 2012. I’ll leave discussions on restrictive diets for another post coming up and let’s get back to all the “morbidly obese” that have our societies so traumatized, terrified and also condescendingly didactic all at once.
What Peter Attia Gets Right
The increasing size of the fat organ in response to the onset of metabolic chronic illness is likely a health protective mechanism.
The increasing size of the fat organ in response to the onset of metabolic chronic illness is likely a health protective mechanism.
Yes, I meant to repeat that sentence. Let it sink in for a moment.
Who is Dr. Peter Attia?
He is a physician who developed diabetes despite being incredibly fit and average-weighted at the time. That humbling experience has spurred him on to identify what really causes diabetes mellitus. Although he falls prey to the same mistake we all do of presuming that the treatment for insulin resistance also will ensure the prevention of the onset of the condition, he is nonetheless keen to allow himself to be taken where the science goes.
A fat organ that is capable of increasing in size in response to various stressors is more health and life protective than a fat organ that is less capable of increasing in size. This fact is wrongly referred to as the “obesity paradox*”.
*obviously there is no “paradox” when you understand that obesity is not a life-limiting condition or disease of any kind.
Various stressors might cause the fat organ to have to increase in size to protect your life: persistent insomnia, unrelenting and out-of-your-control stress, various prescription drugs impacting either pulse rates and/or levels of various reproductive, digestive, and/or metabolic hormones, the exposure to various endocrine disruptors in everyday hygiene, make-up and household products, various disease states and of course unknown genetic predispositions as well.
Restriction of food intake is a monstrous stressor. However, although the time span is variable, the fat organ will usually return to its optimal heritable size when the stressors that caused it to have to work harder (and increase in size) resolve.
Fat is the largest hormone-producing organ in your body. The size or increase-in-size of the fat organ is not correlated to food intake or activity levels. You'll need to read Weight Gain Correlates in Literature Part 1 and 2 if you need the definitive science on those facts.
Yet we still cling to the idea that we just need to “eat healthy” and “get out more” and that’s that.
In other words, people with diabetes and/or cardiovascular disease, don’t have those conditions because they are fat.
The causes of the onset of those metabolic conditions are largely unknown and most certainly multivariate, but the increase in size in the fat organ in response to the presence of such a condition appears to happen in an effort to try modulate and alleviate the impact of the metabolic condition on the body.
That’s why fat people with metabolic chronic illness are less likely to die than average-weighted people with the same metabolic chronic illness. 57,58,59
But Wait! How Many of Us Are Actually Sick Anyhow?
To hear the medical industrial complex tell it, we are all ticking time bombs. Millions of us are walking around with absolutely no symptoms— a silent disease (or several) lurking within us that, if only caught early enough, will be neutralized so that we might realize the immortal and healthy lives we are owed.
We are just one screening test away from having our mortal selves transcended utterly and completely.
As Nortin Hadler notes in his book Worried Sick: A Prescription for Health in an Overtreated America, the “public-health world is alarming us about yet another epidemic that the public-health world itself is creating by virtue of changing the rules for labeling.” (p.48)
And these epidemics are not of disease states, they are of risk factors identified by changing cut-off points alone.
Screening an asymptomatic well person for disease is not the same as applying diagnostic testing to a symptomatic sick person.
Screening an asymptomatic well person may identify a risk factor.
Applying diagnostic tests to a symptomatic sick person may identify the underlying disease.
A risk factor is not a disease.
I have celiac disease and presumably several of my relatives who do not have the disease, may have the genetic risk factor. Critically, they can eat gluten and I cannot. And eating gluten will not turn that risk factor into the disease for my asymptomatic relatives either.
Have high-blood pressure? Not a disease.
Have sleep apnea? Not a disease.
Have poor cholesterol levels or ratio? Not a disease.
Have bad fasting blood glucose levels? Not actually a disease.
Have polyps in the colon? Not a disease.
Have plaque build-up in the arteries? Not a disease.
Have high intraocular pressure? Not a disease.
The above are all risk factors in the same way as the genotype for gluten-sensitive enteropathy is a risk factor for developing celiac disease. Many will live out their lives with the above risk factors never developing into a disease state. And with newer more aggressive cut-off points, the argument that there is actually a measurable risk factor present is just that— merely an argument and not evidence-based medicine.
Do you screen for disease in the absence of symptoms? And then do you treat a risk factor? Well that’s entirely up to you, but I won’t. I won’t because there are no compelling data that such intervention actually removes the risk of the possible anticipated disease in future. And there are reasonable data that such treatments are going to cause more harm than leaving well enough alone.
Edited to add:
When this post was first published, one person was kind enough to comment on the above paragraph to let me know that she hoped I got cancer and died — ah, the internet.
All this is by way of pointing out that a huge amount of the information you have read about the deadliness of obesity as it relates to weakly correlated disease states is actually based on risk factor identification and not even disease. Furthermore, the risk factors are themselves becoming weaker and weaker in context, as the cut-off points are progressively lowered.
You Are Being Conned
In 1992, the Synar Ammendment was enacted by the US Congress to require that states enact laws prohibiting the sale of tobacco to minors. 60
The tobacco conglomerates finally found decades' worth of marketing manipulation and suppression of clinical data unraveled to the point where it became difficult to hide that cigarettes unequivocally contribute to a host of illnesses and cancers. At that point many states in the United States decided to sue tobacco companies for health care reimbursement costs. These litigations were successful and many states were recipients of significant payouts.
In 1997, then Governor of the State of Florida, Lawton Chiles, decided to apply some settlement monies towards an effort to try to stem the ever-increasing smoking rates found amongst youth in that state.
The linchpin of the project was the Florida Youth Tobacco Survey with a representative sample of over 22,000 middle and high school students across the state.
With feedback and input from the Students Working Against Tobacco (SWAT) chapters that were set up across the state, the marketing director of that program (then 18-year-old Jared Perez) determined that the $25 million advertising budget would focus on how teens were being lied to by the tobacco industry, rather than spelling out the usual health consequences of taking up smoking. It was called the “truth” campaign and the annual survey monitored its success.
“By the end of the first year, each measure of tobacco use behavior was significantly lower in Florida than the nation.” 61
After just one year, tobacco use dropped by 19% for middle school students and 8% for high school students in Florida. 62
But in 1998, a $206 billion annual settlement with major tobacco companies occurred. This was the master settlement between Philip Morris, RJ Reynolds, Brown & Williamson and Lorillard and 46 states, allowing for the tobacco industry to avoid a state-by state litigation and settlement process. However, that settlement requires that the companies not be “vilified” in any anti-smoking advertisements. 63
Needless to say the Florida “truth” campaign was neutralized as its entire focus had been to let teens know they were being lied to by the tobacco industry. That emphasis most certainly “vilified” the industry and was therefore going to risk counter-litigation by the tobacco industry to force “anti-vilification” compliance.
“It is difficult to get a man to understand something, when his salary depends upon his not understanding it.” — Upton Sinclair
But That Was The Evil Tobacco Industry
“Finance Director of Weight Watchers explained that it’s the ‘perfect business model,’ because people are doomed to fail.” 64
So let’s say I say to you “You’re fat and to get healthy you have to lose weight.”
Your first question to me should be: “Who the hell are you?” and not “Oh my god, how do I lose weight now?”
The weight loss industry reaped an estimated $61 billion in the US and $180 billion worldwide in 2012. 65 In the same year, by comparison, the tobacco industry generated sales of $491 billion worldwide but only $35 billion in the US. 66
In other words, the weight loss industry in the US now pulls in double the revenue of the tobacco industry in that same country.
You’ll also be happy to know that forecasts suggest that the North American weight loss management market is expected to increase to $139.5 billion by 2017. 67
Just try to find a peer-reviewed published study that indicates obesity is a contributory cause of X or Y disease wherein the researchers are not affiliated in some way to that weight loss industry (that includes, by the way, pharmaceutical options as well as surgeries in addition to things you might equate more readily with the industry like Weight Watcher’s or Jenny Craig).
Upton Sinclair most certainly uttered a timeless observation that has turned out to be far from an industry-specific truism.
Recap
- Your body has its own inherited height, weight and body mass index. It’s yours and tell people that you own it outright. If it’s under construction right now thanks to recovery, then it knows where it’s heading and just leave it alone to do its job.
- The “theory” in weight set point theory is the unproven ways in which the body keeps its weight stable, not that we don't know if it keeps it stable (it does).
- We are a bit heavier, taller and live longer now. Celebrations are a reasonable way to acknowledge these facts.
- The words “overweight” and “obese” are not synonyms for “sick and dying” or “ooo, probably going to get sick very soon if you don’t do something now!”
- The POO exercised poetic forms of interpretation (or possibly financial interest) to say that a point to the right of the peak of the BMI bell curve graph predicts increased levels of illness and premature death. They are out there dancing with sparklers on that one – no evidence to be had.
- “Obesity” is so not a disease that even putting the two words in the same sentence makes me want to disinfect this entire post with a scrub brush and lye.
- Metabolic chronic conditions are present in people who are below average, average and above average weight.
- If a metabolic chronic condition does appear, then a body that responds by getting fatter has generated both a health and life protective response. And that body has better morbidity and mortality outcomes too.
- Many things that are billed as metabolic disease are actually rather nebulous risk factors with ever more questionable cut-off points as well.
- Treating risk factors is popular with the medical industrial complex, but in almost all cases there is no proof it offers the actual sought after preventative outcome (namely that the disease will not manifest down the line).
- While the tobacco industry is considered in a class on its own when it comes to super villainy, it’s unwise to end up living out that oft repeated quote: “Those that fail to learn from history, are doomed to repeat it.” (presumably Winston Churchill).
Now the next section is really just an addendum that is not necessary reading at all. If you stop here, you have practically everything you need to know about weight and obesity that is scientifically known to date.
Skepticism Is A Practice
The ultra-detailed among you will have noticed I mentioned intraocular pressure (IOP) in the list of things that are not diseases, but rather risk factors for disease.
Well, that’s one where it turns out I had to admit to still being a novice skeptic despite years of dedicated practice and commitment. Just the mere act of practicing skepticism is a practice in humility.
I am currently reading Alan Cassels most recent book: Seeking Sickness: Medical Screening and the Misguided Hunt for Disease. As you know his previous book, co-written with Ray Moynihan, is already listed in suggested reading on this site (Selling Sickness). Well, I begin in chapter one feeling self-satisfied with how much I already know as Cassels reviews the questionable value of full CT body scans. “Hmm, yes. So true! How clever is this author clearly, as I wholeheartedly agree and he reflects admirably my own great brain reasoning,” I think to myself.
Then I hit chapter two “Screening for Eyeball Pressure”. I think I can best describe the response as follows: first, a slow increase in intentional focus and curiosity…
Ever had an eye exam where they puff a bit of air at your eyeballs? It’s called air-puff tonometry and it is designed to identify intraocular pressure.
And thanks to many public service announcements (at least in Canada) we likely all know that this test prevents glaucoma.
Ah yes, well it doesn’t prevent glaucoma. And it does not detect glaucoma either. It detects high intraocular pressure that is a risk factor for one kind of glaucoma: open angle glaucoma. 50% of all glaucoma cases do not include high intraocular pressure as a symptom. And not all incidences of high intraocular pressure progress to glaucoma either.
Glaucoma is damage to the optic nerve that usually leads to progressive and irreversible vision loss. Only 0.6% of the US population has glaucoma and of those only 6% are functionally blind. Treatment, depending on the form of glaucoma, involves medications and surgeries to prevent further vision loss.
Now here’s the thing, I’ve had the tonometry test. I did so without even knowing ahead of time what a positive result might then involve for me. That’s a big no-no. Never undergo screening as an asymptomatic individual with no accompanying risk factors unless you know what a positive result might involve.
High intraocular pressure can be misdiagnosed due to operator error and can appear for fleeting reasons such as atmospheric and temperature changes. 68 Prescription eye drops are used to treat high intraocular pressure but side effects include changes in eye color, blurred vision, redness, stinging, itching and burning. And in rare cases patients can even experience a decrease in blood pressure, memory problems and kidney stones. 69
My tonometry test was negative. But had it been positive I would not have known nearly enough to identify that I would be treating a risk factor. And like most risk factors, it might not ever develop into a disease state and yet the treatment of the risk factor might have harmed me.
Everyone needs to know those odds ahead of time even if each individual might make different decisions when faced with the choice of treating a risk factor that may or may not develop into a disease state.
…And we wrap up my unintentional learning moment with a final realization:
Common nonsense seeps into our brains because we do not live hermetically sealed away from our society. So don’t forget to ask yourself first whether you know what you know, or whether you just think you do. Be skeptical of yourself.
1. Girardier, L. "[Autoregulation of body weight and body composition in man. A systematic approach through models and simulation]." Archives internationales de physiologie, de biochimie et de biophysique 102, no. 4 (1993): A23-35.
2. Xu, Yong, Juli E. Jones, Daisuke Kohno, Kevin W. Williams, Charlotte E. Lee, Michelle J. Choi, Jason G. Anderson et al. "5-HT 2C Rs expressed by pro-opiomelanocortin neurons regulate energy homeostasis." Neuron 60, no. 4 (2008): 582-589.
3. Hillebrand, J. J. G., D. De Wied, and R. A. H. Adan. "Neuropeptides, food intake and body weight regulation: a hypothalamic focus." Peptides 23, no. 12 (2002): 2283-2306.
4. Barsh, Gregory S., I. Sadaf Farooqi, and Stephen O'Rahilly. "Genetics of body-weight regulation." Nature 404, no. 6778 (2000): 644-651.
5. Barsh, Gregory S., and Michael W. Schwartz. "Genetic approaches to studying energy balance: perception and integration." Nature Reviews Genetics 3, no. 8 (2002): 589-600..
6. Berthoud, Hans-Rudolf. "Multiple neural systems controlling food intake and body weight." Neuroscience & Biobehavioral Reviews 26, no. 4 (2002): 393-428.
7. D. Joe Millward and D. G. N. G. Wijesinghe, “Energy partitioning and the regulation of body weight–Reply by Millward & Wijesinghe,” British Journal of Nutrition 79, no. 1 (1998): 111-113.
8. R. Cancello, A. Tounian, Ch Poitou, and K Clément, “Adiposity signals, genetic and body weight regulation in humans,” Diabetes & Metabolism 30, no. 3 (2004): 215-227.
9. Hans-Rudolf Berthoud, “Multiple neural systems controlling food intake and body weight,” Neuroscience & Biobehavioral Reviews 26, no. 4 (2002): 393-428.
10. Joel K. Elmquist, Roberto Coppari, Nina Balthasar, Masumi Ichinose, and Bradford B. Lowell, “Identifying hypothalamic pathways controlling food intake, body weight, and glucose homeostasis,” The Journal of Comparative Neurology 493, no. 1 (2005): 63-71.
11. Stunkard, Albert J., Terryl T. Foch, and Zdenek Hrubec. "A twin study of human obesity." Jama 256, no. 1 (1986): 51-54.
12. Harris, Ruth Babette. "Role of set-point theory in regulation of body weight." The FASEB Journal 4, no. 15 (1990): 3310-3318.
13. Ravussin, Yann, Rudolph L. Leibel, and Anthony W. Ferrante. "A missing link in body weight homeostasis: the catabolic signal of the overfed state." Cell metabolism 20, no. 4 (2014): 565-572.
14. Camps, Stefan GJA, Sanne PM Verhoef, and Klaas R. Westerterp. "Weight loss, weight maintenance, and adaptive thermogenesis." The American journal of clinical nutrition 97, no. 5 (2013): 990-994.
15. Camps, S. G., S. P. Verhoef, and K. R. Westerterp. "Leptin and energy restriction induced adaptations in resting energy expenditure and physical activity." How humans economize (2015): 79.
16. Schwartz, Michael W., Stephen C. Woods, Randy J. Seeley, Gregory S. Barsh, Denis G. Baskin, and Rudolph L. Leibel. "Is the energy homeostasis system inherently biased toward weight gain?." Diabetes 52, no. 2 (2003): 232-238.
17. Schwartz, Michael W., Stephen C. Woods, Daniel Porte, Randy J. Seeley, and Denis G. Baskin. "Central nervous system control of food intake." Nature 404, no. 6778 (2000): 661-671.
18. Mizuno, Tooru M., Hideo Makimura, and Charles V. Mobbs. "The physiological function of the agouti-related peptide gene: the control of weight and metabolic rate." Annals of medicine 35, no. 6 (2003): 425-433.
19. Garner, David M., and Susan C. Wooley. "Confronting the failure of behavioral and dietary treatments for obesity." Clinical Psychology Review 11, no. 6 (1991): 729-780.
20. French, Simone A., and Robert W. Jeffery. "Consequences of dieting to lose weight: effects on physical and mental health." Health Psychology 13, no. 3 (1994): 195.
21. Krowchuk, Daniel P., Shelley R. Kreiter, Charles R. Woods, Sara H. Sinal, and Robert H. DuRant. "Problem dieting behaviors among young adolescents." Archives of pediatrics & adolescent medicine 152, no. 9 (1998): 884-888.
22. Neumark-Sztainer, Dianne, Melanie Wall, Jia Guo, Mary Story, Jess Haines, and Marla Eisenberg. "Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later?." Journal of the American Dietetic Association 106, no. 4 (2006): 559-568.
23. Wing, Rena R., and James O. Hill. "Successful weight loss maintenance." Annual review of nutrition 21, no. 1 (2001): 323-341.
24. Anderson, James W., Elizabeth C. Konz, Robert C. Frederich, and Constance L. Wood. "Long-term weight-loss maintenance: a meta-analysis of US studies." The American journal of clinical nutrition 74, no. 5 (2001): 579-584.
25. Curioni, C. C., and P. M. Lourenco. "Long-term weight loss after diet and exercise: a systematic review." International journal of obesity 29, no. 10 (2005): 1168-1174.
26. Jeffery, Robert W., Leonard H. Epstein, G. Terence Wilson, Adam Drewnowski, Albert J. Stunkard, and Rena R. Wing. "Long-term maintenance of weight loss: current status." Health psychology 19, no. 1S (2000): 5.
27. Sjöström, Lars, Aila Rissanen, Teis Andersen, Mark Boldrin, Alain Golay, Hans PF Koppeschaar, Michel Krempf, and European Multicentre Orlistat Study Group. "Randomised placebo-controlled trial of orlistat for weight loss and prevention of weight regain in obese patients." The Lancet 352, no. 9123 (1998): 167-172.
28. Turk, Melanie Warziski, Kyeongra Yang, Marilyn Hravnak, Susan M. Sereika, Linda J. Ewing, and Lora E. Burke. "Randomized clinical trials of weight-loss maintenance: A review." The Journal of cardiovascular nursing 24, no. 1 (2009): 58.
29. Wadden, Thomas A., Leslie G. Womble, David B. Sarwer, Robert I. Berkowitz, Vicki L. Clark, and Gary D. Foster. "Great expectations:" I'm losing 25% of my weight no matter what you say"." Journal of consulting and clinical psychology 71, no. 6 (2003): 1084.
30. Stern, Linda, Nayyar Iqbal, Prakash Seshadri, Kathryn L. Chicano, Denise A. Daily, Joyce McGrory, Monica Williams, Edward J. Gracely, and Frederick F. Samaha. "The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial." Annals of internal medicine 140, no. 10 (2004): 778-785.
31. Schwartz, Michael W., and Randy J. Seeley. "The new biology of body weight regulation." Journal of the American Dietetic Association 97, no. 1 (1997): 54-58.
32. Zoico, E., M. Zamboni, V. Di Francesco, G. Mazzali, F. Fantin, G. De Pergola, A. Zivelonghi, S. Adami, and O. Bosello. "Relation between adiponectin and bone mineral density in elderly post-menopausal women: role of body composition, leptin, insulin resistance, and dehydroepiandrosterone sulfate." Journal of endocrinological investigation 31, no. 4 (2008): 297-302.
33. Newman, Anne B., Jung Sun Lee, Marjolein Visser, Bret H. Goodpaster, Stephen B. Kritchevsky, Frances A. Tylavsky, Michael Nevitt, and Tamara B. Harris. "Weight change and the conservation of lean mass in old age: the Health, Aging and Body Composition Study." The American journal of clinical nutrition 82, no. 4 (2005): 872-878.
34. Hughes, Virginia A., Walter R. Frontera, Ronenn Roubenoff, William J. Evans, and Maria A. Fiatarone Singh. "Longitudinal changes in body composition in older men and women: role of body weight change and physical activity." The American journal of clinical nutrition 76, no. 2 (2002): 473-481.
35. Gurven, Michael, and Hillard Kaplan. "Longevity among hunter‐gatherers: a cross‐cultural examination." Population and Development review 33, no. 2 (2007): 321-365.
36. Gurven, Michael, Hillard Kaplan, and Maguin Gutierrez. "How long does it take to become a proficient hunter? Implications for the evolution of extended development and long life span." Journal of human evolution 51, no. 5 (2006): 454-470.
37. Armelagos, George J., Alan H. Goodman, and Kenneth H. Jacobs. "The origins of agriculture: Population growth during a period of declining health." Population and Environment 13, no. 1 (1991): 9-22.
38. Mummert, Amanda, Emily Esche, Joshua Robinson, and George J. Armelagos. "Stature and robusticity during the agricultural transition: evidence from the bioarchaeological record." Economics & Human Biology 9, no. 3 (2011): 284-301.
39. Filozof, C., Fernandez Pinilla, and A. Fernández‐Cruz. "Smoking cessation and weight gain." Obesity reviews 5, no. 2 (2004): 95-103.
40. Aubin, Henri-Jean, Amanda Farley, Deborah Lycett, Pierre Lahmek, and Paul Aveyard. "Weight gain in smokers after quitting cigarettes: meta-analysis." (2012): e4439.
41. Williamson, David F., Jennifer Madans, Robert F. Anda, Joel C. Kleinman, Gary A. Giovino, and Tim Byers. "Smoking cessation and severity of weight gain in a national cohort." New England Journal of Medicine 324, no. 11 (1991): 739-745.
42. McPherson, Kitta, Edward R. Silverman, “Obesity: Fat pills, fat profits,” Feb 16, 1997, p.1, “Fat’s Overlap,” Feb. 17, 1997, p.1, Star Ledger Special.
43. Eaton, William W., Haroutune Armenian, Joseph Gallo, Laurie Pratt, and Daniel E. Ford. "Depression and risk for onset of type II diabetes: a prospective population-based study." Diabetes care 19, no. 10 (1996): 1097-1102.
44. Hafeezullah, Adnan Mahmood Gul, and Abdul Hadi. "Prevalence of Diabetes Mellitus Among Obese And Non-obese Patients With Coronary Artery Disease." J Ayub Med Coll Abbottabad 22, no. 3 (2010).
45. Kashima, Saori, Kazuo Inoue, Masatoshi Matsumoto, and Kimihiko Akimoto. "Prevalence and characteristics of non‐obese diabetes in Japanese men and women: the Yuport Medical Checkup Center Study." Journal of diabetes 7, no. 4 (2015): 523-530.
46. Prando, Romano, Valeria Cheli, Pierluigi Melga, Roberta Giusti, Emanuela Ciuchi, and Patrizio Odetti. "Is Type 2 Diabetes a Different Disease in Obese and Nenobese Patients?." Diabetes Care 21, no. 10 (1998): 1680-1685.
47. Hainer, Vojtech, and Irena Aldhoon-Hainerová. "Obesity paradox does exist." Diabetes care 36, no. Supplement 2 (2013): S276-S281.
48. Woolf, STEVEN H., and STEPHEN F. Rothemich. "New diabetes guidelines: a closer look at the evidence." American family physician 58, no. 6 (1998): 1287.
49. Mortimore, I. L., I. Marshall, P. K. Wraith, R. J. Sellar, and N. J. Douglas. "Neck and total body fat deposition in nonobese and obese patients with sleep apnea compared with that in control subjects." American journal of respiratory and critical care medicine 157, no. 1 (1998): 280-283.
50. Applegate, William B., Jeff P. Hughes, and Roger Vander Zwaag. "Case-control study of coronary heart disease risk factors in the elderly." Journal of clinical epidemiology 44, no. 4 (1991): 409-415.
51. McGill, H.C., ARIASSTE. J, CARBONEL. LM, Correa, P., DeVeyra, E.A., Donoso, S., Eggen, D.A., Galindo, L., Guzman, M.A., LICHTENB. E and Loken, A.C., 1968. General Findings of international Atherosclerosis project. Laboratory Investigation, 18(5), p.498.
52. Flegal, Katherine M., Barry I. Graubard, David F. Williamson, and Mitchell H. Gail. "Excess deaths associated with underweight, overweight, and obesity." Jama 293, no. 15 (2005): 1861-1867.
53. Hursting, Stephen D., Nomeli P. Nunez, Lyuba Varticovski, and Charles Vinson. "The obesity-cancer link: lessons learned from a fatless mouse." Cancer Research 67, no. 6 (2007): 2391-2393.
54. Calle, Eugenia E., Carmen Rodriguez, Kimberly Walker-Thurmond, and Michael J. Thun. "Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults." New England Journal of Medicine 348, no. 17 (2003): 1625-1638.
55. Griggs, Jennifer J., Melony ES Sorbero, and Gary H. Lyman. "Undertreatment of obese women receiving breast cancer chemotherapy." Archives of internal medicine 165, no. 11 (2005): 1267-1273.
56. Wildman, Rachel P., Paul Muntner, Kristi Reynolds, Aileen P. McGinn, Swapnil Rajpathak, Judith Wylie-Rosett, and MaryFran R. Sowers. "The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004)." Archives of internal medicine 168, no. 15 (2008): 1617-1624.
57. Oga, Emmanuel Aja, and Olabimpe Ruth Eseyin. "The Obesity Paradox and Heart Failure: A Systematic Review of a Decade of Evidence." Journal of obesity 2016 (2016).
58. Hainer, Vojtech, and Irena Aldhoon-Hainerová. "Obesity paradox does exist." Diabetes care 36, no. Supplement 2 (2013): S276-S281.
59. Park, Jongha, Seyed-Foad Ahmadi, Elani Streja, Miklos Z. Molnar, Katherine M. Flegal, Daniel Gillen, Csaba P. Kovesdy, and Kamyar Kalantar-Zadeh. "Obesity paradox in end-stage kidney disease patients." Progress in cardiovascular diseases 56, no. 4 (2014): 415-425.
60. DiFranza, Joseph R., and G. F. Dussault. "The federal initiative to halt the sale of tobacco to children—the Synar Amendment, 1992–2000: lessons learned." Tobacco Control 14, no. 2 (2005): 93-98.
61. Sly, David F., Gary R. Heald, and Sarah Ray. "The Florida “truth” anti-tobacco media evaluation: design, first year results, and implications for planning future state media evaluations." Tobacco Control 10, no. 1 (2001): 9-15.
62. http://legislature.vermont.gov/assets/Documents/2016/WorkGroups/Senate%20Appropriations/FY%202016%20Budget/11%20Public%20Hearings-Public%20Testimony/W~none~Blueprint%20for%20a%20Tobacco%20Free%20VT%20Public%20Hearing%20via%20VIT~2-10-2015.pdf
63. Ibrahim, J. K., and Stanton A. Glantz. "Tobacco industry litigation strategies to oppose tobacco control media campaigns." Tobacco control 15, no. 1 (2006): 50-58.
64. http://www.bbc.co.uk/programmes/b038913v/episodes/guide
65. http://www.prweb.com/releases/2013/4/prweb10629316.htm
66. https://www.theguardian.com/business/2012/mar/22/tobacco-profits-deaths-6-million
67. http://www.marketsandmarkets.com/PressReleases/north-america-weight-loss-obesity-management.asp
68. Van de Veire, Sara, Peter Germonpre, Charlotte Renier, Ingeborg Stalmans, and Thierry Zeyen. "Influences of atmospheric pressure and temperature on intraocular pressure." Investigative ophthalmology & visual science 49, no. 12 (2008): 5392-5396.
69. Falsini, Benedetto, Dario Marangoni, Tommaso Salgarello, Giovanna Stifano, Lucrezia Montrone, Salvatore Di Landro, Laura Guccione, Emilio Balestrazzi, and Alberto Colotto. "Effect of epigallocatechin-gallate on inner retinal function in ocular hypertension and glaucoma: a short-term study by pattern electroretinogram." Graefe's Archive for Clinical and Experimental Ophthalmology 247, no. 9 (2009): 1223-1233.